- (212) 686-6066
- Mon - Sat: 7am - 8pm
- Sun: 9am - 5pm

Parkmed NYC specializes in fibroid management and outpatient treatment. Our board-certified physicians are experts at evaluating and treating patients with fibroids using all of the available techniques and combinations with the most up-to-date therapies and medications. We understand that each patient’s concerns are different and their treatment has to be individually designed. Because fibroids come in all sizes and exist in different parts of the pelvis, symptoms can vary greatly from one patient to the next. During your visits, we will do your full evaluation, sonogram, and laboratory work as well as review all the appropriate treatments with you as we generate a plan together.
We maintain two operative suites and we perform a multitude of procedures for fibroid treatment without the need for referral to a hospital including:
If necessary, our physicians also perform laparoscopy, minimally-invasive surgery, and robotic-assisted surgery at NYU Langone Medical Center or Mount Sinai Hospital. Our facility will take care of your insurance approvals, pre-operative evaluation, and schedule your surgery with one of our physicians at the hospital.
Whether you’ve been told that you have fibroids, are concerned about your symptoms, need a second opinion for surgery, or just want to plan a safe pregnancy, give us a call and make an appointment for your consultation today!
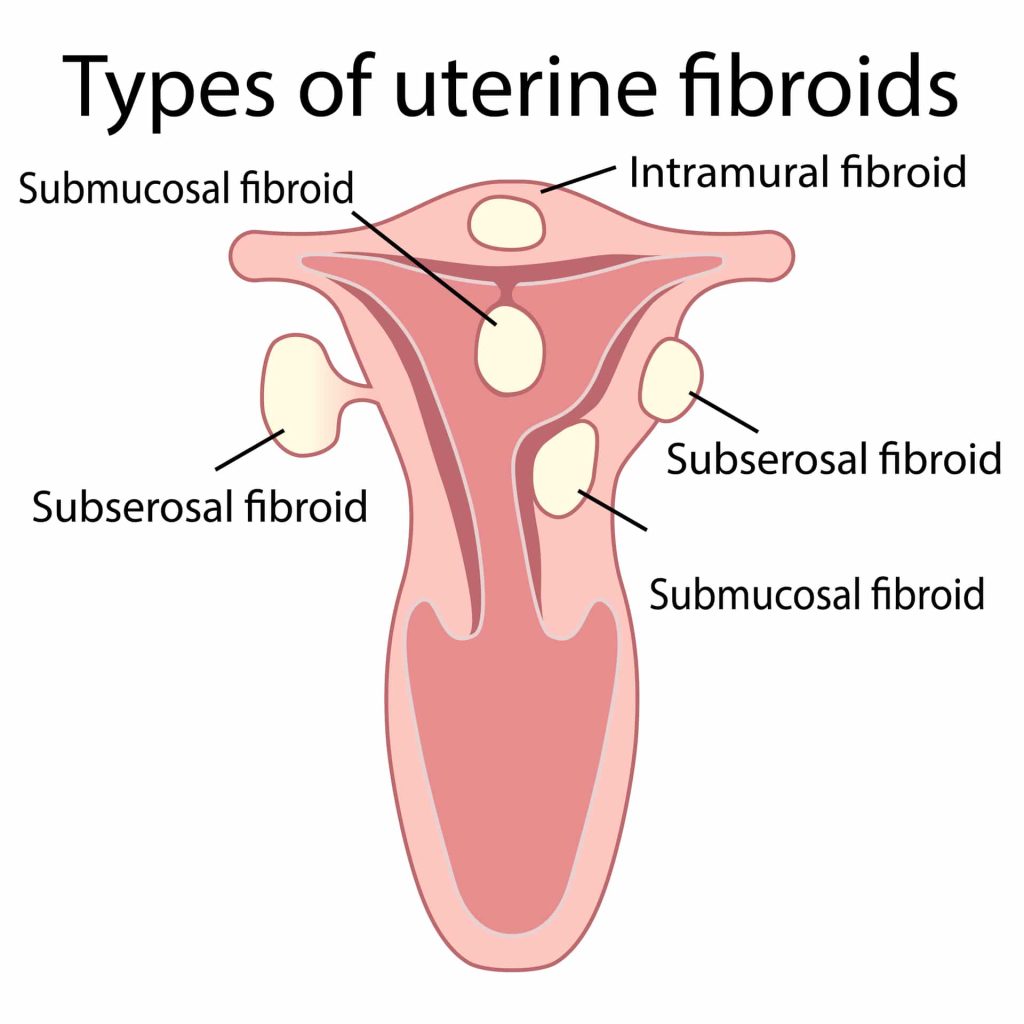
Uterine fibroids are benign (not cancerous) growths that develop from the muscle tissue of the uterus. They also are called leiomyomas or myomas. The size, shape, and location of fibroids can vary greatly. They may be present inside the uterus, on its outer surface or within its wall, or attached to it by a stem-like structure. A person may have only one fibroid or many of varying sizes. A fibroid may remain very small for a long time and suddenly grow rapidly, or grow slowly over a number of years.
Changes in your menstruation (abnormal uterine bleeding)
Pain
Pregnancy complications
Fibroids can break down (degeneration) and cause pain, nausea, vaginal infections or fevers, but they can also grow rapidly and cause abdominal swelling. Fibroids also may cause infertility, and can complicate pregnancies and cause difficulty with prenatal care and delivery. When fibroids are thought to affect fertility or complicate a pregnancy, many women undergo treatment first, and then are able to become pregnant after they are treated.
Fibroids are almost always benign. Rarely will a cancerous fibroid occur. Having fibroids does not increase your chances of any other cancer.
The first step to diagnosing fibroids is a thorough history and physical exam, including a pelvic exam. Based on your symptoms, your provider will usually request a pelvic or transvaginal ultrasound to evaluate the uterus and visualize any fibroids. Ultrasounds are machines that use soundwaves to evaluate pelvic organs. They are performed the same day as your visit, at your bedside with trained sonographers at Parkmed NYC, and without need for a referral to an outside radiology center. This ultrasound is a quick and thorough assessment of your uterine cavity, ovaries and fallopian tubes, and can also detect fibroids, polyps, and any other gynecologic pathology. Based on the initial findings, your physician may recommend additional imaging which may include:
Saline Infusion Sonography (SIS): A test in which fluid is put into the uterus through the cervix and ultrasonography is then used to show the inside of the uterus. This is useful for diagnosis of polyps and submucosal fibroids.
Hysteroscopy uses a camera device (hysteroscope) is inserted through the vagina and cervix, and used to directly visualize fibroids the inside of the uterus. It can also detect polyps, abnormal uterine shape and abnormal tissue.
Hysterosalpingography: A special X-ray test done at a radiology center that detects abnormal changes in the size and shape of the uterus and fallopian tubes.
Laparoscopy uses a camera device (the laparoscope) that is inserted through a small cut just below or through the navel (belly button) to allow the doctor to see the inside of the abdomen and fibroids on the outside of the uterus.
CT Scan/MRI: These are imaging techniques done at a radiology center to visualize the details of your uterus and fibroids. They are used as a part of your surgical planning for complicated procedures, or to evaluate for cancer.
At Parkmed NYC we perform our own ultrasonography, SIS and hysteroscopy at the office. If we feel that you may need additional detailed imaging, we will take care of your referrals and insurance approvals to any of our associated local radiology centers.
Certain signs and symptoms may signal the need for treatment:
Fibroids that do not cause symptoms, are small, or occur in an individual who is nearing menopause often do not require treatment, but should be monitored with ultrasonography as recommended by your physician.
Medical drugs and surgical options both exist for fibroids. Different patients will require different approaches for the treatment of their fibroids. It is important that each patient is individually assessed and that a treatment regimen is tailored specifically for them and the alleviation of their particular symptoms. Treatment is often dependent on the location of your fibroid, and the symptoms that you are experiencing. Certain medications may reduce the heavy bleeding and painful periods that fibroids cause, but they may not prevent the growth of fibroids. Surgery often is needed as well. Drug treatment for fibroids includes the following options:
Various surgeries can be performed to alleviate symptoms, shrink fibroids, or to remove fibroids, depending on the goal that you and your provider have agreed on.
Hysteroscopy: used to remove submucosal fibroids that are inside the cavity of the uterus. Often, an instrument called a resectoscope is used.
Endometrial Ablation: used to destroy the lining of the uterus to alleviate heavy bleeding. This can also be done selectively to reduce vasculature and shrink fibroids.
Myomectomy: the surgical removal of fibroids while leaving the uterus in place. Fibroids do not regrow after surgery, but new fibroids may develop. If they do, more surgery may be needed.
Hysterectomy: the removal of the uterus. Hysterectomy is done when other treatments have not worked or are not possible or the fibroids are very large and a woman is no longer planning to have children.
Uterine Artery Embolization (UAE): A technique that cuts off blood flow to the uterus to shrink the fibroid—this is usually reserved for patients who are too high risk or not candidates for other surgeries.
Myomectomies and hysterectomies can be performed using a variety of techniques. Most fibroids can be addressed using a minimally-invasive approach, with few or no incisions on the abdomen. For larger fibroids, your physician may recommend an open technique that may sometimes require a short stay in a hospital.
Having an annual health care visit is a great opportunity to take charge of your health. A well/annual visit provides an excellent opportunity to discuss methods of maintaining a healthy lifestyle and minimizing health risks. Physicians have an opportunity to contribute to your overall health and well-being by providing recommended preventive care and counseling or refer for recommended services. Routine health care visits can help find problems early or prevent health problems before they occur. If problems are found early, they may be easier to treat and less likely to pose serious risks to your health. These assessments should include screening, evaluation/counseling, and immunizations based on age and risk factors.
A key component of a well/annual visit for a reproductive-aged patient is the development and discussion of a reproductive life plan to ensure that medical testing and treatments provided are aligned with the patient’s current and future plans. A discussion of a reproductive life plan may include pre-pregnancy counseling, infertility assessment, or the full range of contraceptive options. Routine screening for gynecological diseases or conditions are equally as important, and periodic well/annual visits are appropriate and necessary for perimenopausal and postmenopausal patients as well.